Home
Subscription
April 2024 issue
April 1, 2024 issue
March 2024 issue
February 2024 issue
January 2024 issue
BACK ISSUES
2023
2022
2021
2020
2019
2018
2017
2016
2015
2014
2013
2012
2011
2010
2009
2008
2007
2006
|
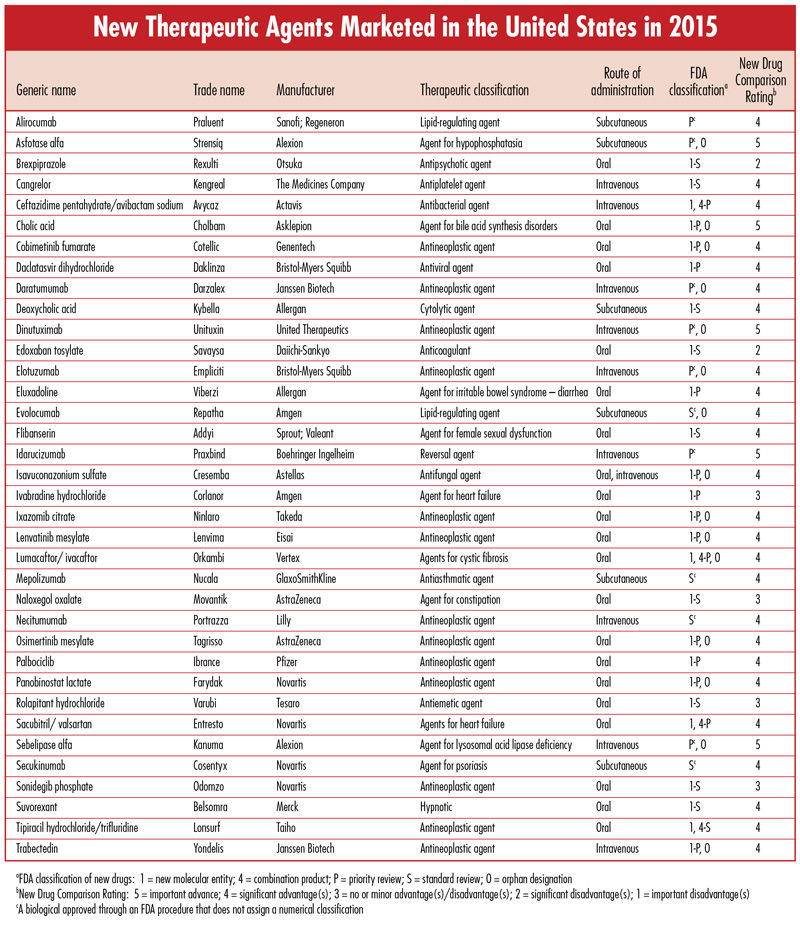
Each issue will include an editorial on a topic that is important for the profession of pharmacy, as well as a review of a new drug that includes a comparison of the new drug with previously marketed drugs that are most similar in activity, and a New Drug Comparison Rating (NDCR) for the new drug. Read on for this month's issue. June 2016 Issue [Download PDF format] In this issue: • Editorial • New Therapeutic Agents Marketed in the United States in 2015 |
|
|
EDITORIAL: Editor's note: There has been extensive ongoing controversy and debate regarding issues or actions having life or death consequences. The most prominent of these issues are abortion, execution via lethal injection, and physician-assisted suicide. Recent news commentaries identify an increased number of abortions in Latin American countries because of concerns about birth defects in babies born to mothers with Zika virus infection, Pfizer's announcement that it will restrict distribution of its medications that are used for lethal injections in executions (although it is noteworthy that Pfizer is silent about the availability of its drug misoprostol [Cytotec] that is used for abortions), and California's legalization of physician-assisted suicide. There is no question that all health professionals will experience increased challenges with respect to their professional, religious, moral, and ethical convictions. The following commentary was written in response to an article by a physician who is an advocate for physician-assisted dying. Although the commentary below was developed for a physician audience, there are many implications for pharmacists who would be requested to provide the pertinent medications. The authors are my son, Eric Hussar, a pharmacist and family practice physician, and his wife, Terra Hussar, a neurologist. Physician-Assisted SuicideCan we not care best for our patients by walking with them in the dying instead of leading them to it?We read with great concern the article on Physician-Assisted Dying. We think we should start by calling this process for what it is. The article mentioned that national support for this action is much greater when it is not referred to as physician-assisted suicide (PAS). Suicide, as defined by the Merriam-Webster Dictionary is: "the act or an instance of taking one's own life voluntarily and intentionally especially by a person of years of discretion and of sound mind." When physicians assist in the process, it is less messy and less dramatic, but it is still suicide. It is the process of a person actively taking his own life with the help of a doctor. This is distinctly different from withdrawing care at the end of life, or using pain medication which may slow the respiratory drive, as the primary purposes of those are not to end life. There are several large problems with PAS, which we will briefly identify below. Before delving into these, however, we wish to state that we do not condemn or judge those in favor of legalizing PAS. We believe that they are interested in the welfare of their patients, and do sincerely care for those whom they deem to be candidates for PAS. But for the reasons that follow, we cannot agree with this practice.Prognosis - Currently Oregon requires that physicians must give a prognosis of a lifespan of 6 months or less to a patient who desires PAS. None of us truly know the future and many people have lived long beyond their predicted life expectancy. Though there may be pain and suffering involved, we could be robbing patients and families of significant amounts of time with each other, which could include very meaningful interaction. Mental Health Concerns - Patients requesting PAS need to be referred for a psychiatric or psychological evaluation if it is felt that they are suffering from depression significant enough to have an impact on their decision. Only 3 of the 105 patients who died by this process last year in Oregon were referred for this evaluation. One could imagine that far many more were affected by depression to a severe enough degree to coax them towards this, but that they did not want to be referred or were not offered that choice. Trust - If PAS is legalized further, trust can be eroded between patients and doctors. Patients may become suspicious of a physician's intentions towards them. Patients with terminal illnesses, or even chronic disabling conditions could be worried that their physician may be leading them to a choice that seems easier for everyone if it brings their difficult life to an end sooner. Pain - While much of what we do in medicine is designed to alleviate pain, the elimination of pain should not be the ultimate goal in healthcare. The ultimate goal should be the promotion of the best physical, emotional and spiritual health possible. Pain is uncomfortable, and it is reasonable to try to help relieve it, but we think all of us can recall painful times in our life where we grew tremendously as a person in the midst of the difficult and even painful times. Pain can often result in the strengthening of relationships, in a stronger spirit, and in the growth of our spiritual character to a point not otherwise attainable without the aforementioned discomfort. Kara Tippetts, a brave wife and mother who victoriously challenged breast cancer even to her early death, stated, "Suffering is not the absence of goodness, it is not the absence of beauty, but perhaps it can be the place where true beauty can be known." God - God has given us life, and it is not our prerogative to decide when to end it, whether for ourselves or for our patients. We may not understand why He allows people to go through certain types of suffering, but we can trust His goodness and love, even in the hard times, and if we turn to Him, we will find the grace and ability to get through it. In the article that has prompted this response, it is noted that the number of people in our country who believe in nothing in particular has risen to 22.8%. This still leaves 77.2% who do believe in God. And even if you believe that there is no God, or that the presence of God should have no effect on our lives, you must follow that to its natural end. Take away God, and you must remove any moral absolute. Killing a terminally ill patient is ok, as is killing a disabled person, a demented person, or perhaps someone who has different beliefs than you do. As Nietzsche, the famous atheist/agnostic, said, "You have your way. I have my way. As for the right way, the correct way, and the only way, it does not exist." Without God, there can be no accuser of ISIS or Hitler. Everyone does what is right in his own eyes, and no one has the right to tell him that it is wrong. The Soul - Though there are many differences of opinion on this as well, many Americans (ourselves included) believe that we all have a soul, and that our soul has an eternal destination. Part of end-of-life care for patients should include discussion about their beliefs on this. Too many times we are completely focused on this life alone as opposed to what will happen afterwards. We believe that as Americans, and especially as health professionals, we are trained for having control. We all face patients for whom we do not have a concrete plan for treatment, do not know how to improve their health, or lack knowledge of what testing will aid in the diagnosis. How much more helpless do we feel when we have a patient with an illness that will likely prematurely end their lives and is causing them physical or emotional pain? All of our medical interventions cannot save this life indefinitely. We recognize that some will wish to achieve or maintain control by using a medical "treatment" that will end it sooner, or at least when a patient no longer wishes to live. We can therefore preserve the illusion of control and power over the disease process with a tool of PAS. There is no doubt we need to better utilize hospice and palliative care services in order to maximize pain management and provide optimal comfort and support to our patients and their families. Yet even these will fall short at times in eliminating pain and suffering, physical and emotional. As mentioned before, and as many dying patients can attest to, God can meet us in our pain and do something beautiful that may not have been possible otherwise. We have not personally had family members or very close friends who have experienced this depth of suffering. We have experienced time with patients in their last days, and enjoyed precious moments with those who were close to death, who were glad that they had not chosen to end their lives earlier, but instead decided to make the most of every moment they had. We also encourage readers to visit two other sites, as they speak in more experienced and personal ways as to why we must keep PAS illegal. The first is from a physician in Oregon, who has seen first-hand the negative effects of PAS in his state, and who also walked alongside his wife of 40 years who lived beyond her prognosis before succumbing to cancer. The second is a letter from Kara Tippetts (quoted above) to Brittany Maynard, the 29 year old who utilized PAS to end her life after being diagnosed with a brain tumor. Please consider these as primary sources relating the imminent dangers inherent in PAS, and the incredible value of every minute of life that we have, even when there is suffering involved. Can we not care best for our patients by walking with them in the dying instead of leading them to it? Recommended related articles: A Doctor-Assisted Disaster for Medicine Dear Brittany: Why We Don't Have To Be So Afraid of Dying & Suffering that We Choose Suicide Eric F. Hussar, M.D.
Susquehanna Family Medicine Marietta, PA Terra L. Hussar, M.D. Department of Neurology Hershey Medical Center Hershey, PA |
|
| |