Home
Subscription
February 2026 issue
January 2026 issue
BACK ISSUES
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
2015
2014
2013
2012
2011
2010
2009
2008
2007
2006
|
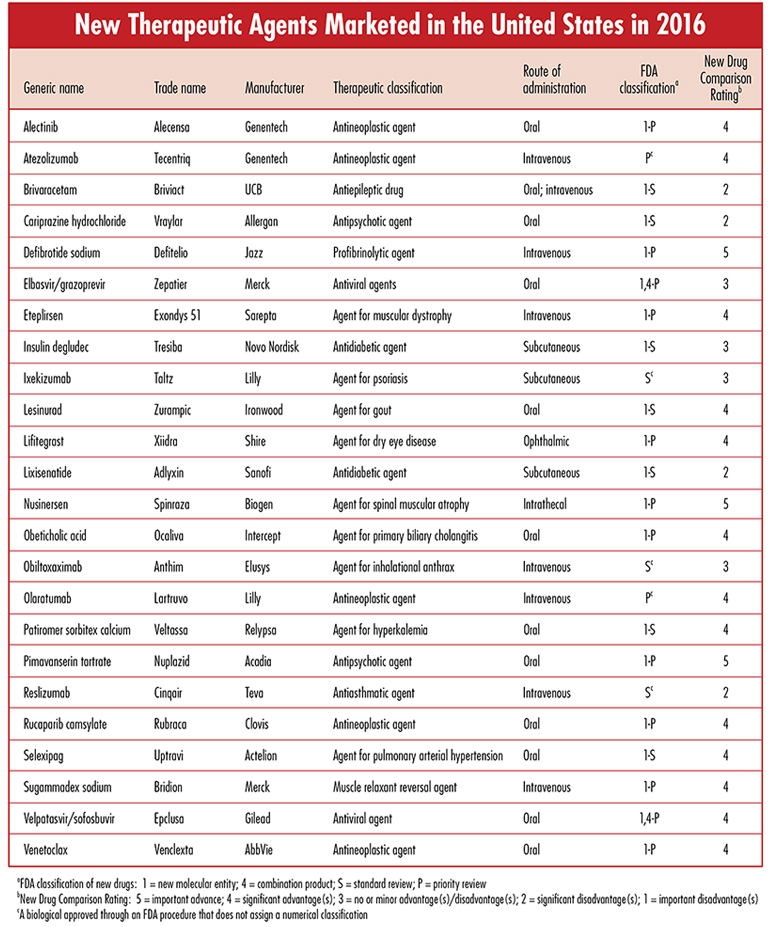
Each issue will include an editorial on a topic that is important for the profession of pharmacy, as well as a review of a new drug that includes a comparison of the new drug with previously marketed drugs that are most similar in activity, and a New Drug Comparison Rating (NDCR) for the new drug. Read on for this month's issue. May 2017 Issue [Download PDF format] In this issue: • Editorial • New Therapeutic Agents Marketed in the United States in 2016 |
|
EDITORIAL:Our Profession's Own Pharmacy Care Administrator (PCA): Can a Dream Become Reality?No other situations have had more of a destructive impact on community pharmacy practice and the provision of pharmacist services to patients than the unfair, oppressive, and non-negotiable terms of pharmacy benefit manager (PBM) prescription programs and their abysmal compensation for pharmacists. The most severe consequences are experienced by independent pharmacists, but many chain pharmacies are also negatively affected. For example, Rite Aid's financial problems are such that its best hope is that it will be acquired by Walgreens. Target, with its extensive and successful retail experience, could not find a way to be financially successful in operating its pharmacies, with the result that it sold them to CVS.Concerns about PBMs and their programs have been the subject of numerous previous editorials in The Pharmacist Activist (for example, please see "Prescription Drug Prices – Billions for Pharmaceutical Companies, Insurance Companies, and PBMs, but Pennies for Pharmacies" [March 2016 issue], "Outrages! – But Some With Opportunities!" [May 2016 issue], and "Understanding and Reducing Drug Prices Must Start with Transparency" [October 2016 issue]). In March I had the opportunity to give a presentation in which I shared some of my "dreams" for the profession of pharmacy, one of which is the following:
"The profession of pharmacy will establish our own prescription drug benefit administration program that provides incentives for achieving positive therapeutic outcomes for patients and equitable compensation for pharmacists, and does not include restricted networks or financial incentives that prevent or discourage continued use of the local pharmacy with which there is a long-term professional relationship and friendship with a personal pharmacist. The current system fragments pharmacist care and increases risk in the use of medications. We can provide a better, safer, and more efficient program.
This "dream" has been a strongly-held opinion of tens of thousands of pharmacists for many years, but the PBM programs have only gone from bad to worse. However, recent events and accusations of pharmaceutical companies, PBMs, and insurance companies against each other have resulted in a greater awareness of the secrecy, manipulation, and deception that characterizes many of the existing prescription benefit programs. Notwithstanding the size, wealth, and political influence of these companies, progressive change is necessary and the time is right for the dream of pharmacy's own pharmacy care administrator (PCA) to become a reality.But can our profession afford such a program? There is a declaration that we have heard often in the last year that can be adapted for our purpose. 'Mexico will pay for the wall.' Our version will be, 'Pharmaceutical companies will pay for this program,' and I would quickly add that it will be in their best interests to do so. After all, it is the drugs they have developed for which we as pharmacists will increase effectiveness and safety, increase societal recognition of the value of medications, and increase the companies' return on their investments." Recent events and accusationsWith the exception of the pharmaceutical companies that establish the prices for medications, almost everyone else is very concerned about the high cost of prescription drugs in the United States. In attempting to defend the prices for their medications, the pharmaceutical companies respond that nobody actually pays those prices because the PBMs and others demand such large rebates and discounts. The PBMs respond by saying the prices the companies charge are so high that they are forced to insist on much lower prices. When the pharmaceutical companies and PBMs are asked the specific amounts of discounts and rebates, both groups respond that the information is proprietary and can't be disclosed. The failure to substantiate accusations with specific information results in the further erosion of credibility of both the pharmaceutical companies and the PBMs. One estimate of the discounts, rebates, etc. is that, on average, they are 44% off the list prices of brand-name drugs. The PBMs claim to pass on most of these "savings" to their clients, but the specifics are a secret and even the clients are significantly restricted in what they can learn from their audits of the PBM they use ("Inside the 'Scorpion Room' Where Drug Price Secrets Are Guarded;" Bloomberg, May 4, 2017, Neil Weinberg and Robert Langreth).The three largest PBMs, Express Scripts, CVS Health, and OptumRx (a unit of United Health) processed approximately 70% of the prescriptions in the United States in 2016. Anthem is one of the largest health insurance companies in the country and it has a 10-year contract with Express Scripts to administer its prescription plans through 2019. However, Anthem has sued Express Scripts for about $15 billion, accusing it of overcharging at a rate of about $3 billion a year during part of the contract period because it was not passing on what Anthem considered to be its share of the "savings" that the PBM had obtained from rebates and discounts from pharmaceutical companies. Express Scripts has recently noted that it does not expect Anthem to continue as a client when the current contract concludes at the end of 2019. Anthem is Express Scripts largest client and accounted for 16% of the prescriptions that the PBM processed in 2016. Although Express Scripts contends that the contract underperformed in its early years, it currently is very profitable for the PBM as noted in the following commentary in the Wall Street Journal (April 26, 2017; p. B16; Charley Grant):
"Regardless of whether Anthem has a legitimate legal claim, there is no doubt that the contract was extraordinarily lucrative for Express Scripts as measured by unit profitability. That metric, reported as earnings before interest, taxes, depreciation, and amortization per prescription filled was $8.39 from the Anthem business in the first quarter. Express Scripts booked just $3.25 per script filled from other customers."
Perhaps such data has been available previously and I was just not aware of it. However, I am shocked by these numbers for processing prescription claims, particularly in the context of how Express Scripts and other PBMs have dictated such low compensation for the pharmacists who maintain the inventories of expensive medications, dispense the medications, and are expected to provide counseling and other services for patients.The profession of pharmacy must no longer tolerate the disrespect and abuse to which we have been subjected. Most previous efforts to persuade, negotiate, and legislate positive changes have resulted in failures and frustration. If anything, we are caught in a downward spiral of exclusion from networks, unjustified fees, reduced compensation, and further loss of autonomy. We don't stand a chance in battles with giant pharmaceutical companies, insurance companies, and PBMs - UNLESS we have a better plan and own the program. The time to do this is NOW, while the pharmaceutical companies, PBMs, and insurance companies are fighting with and suing each other in efforts to determine which is most at fault for the exorbitant prices of medications. Our own pharmacy care administrator (PCA)The profession of pharmacy must continue its advocacy for legislative initiatives that will provide relief from the restrictions and conditions imposed by the PBMs. However, those who oppose our efforts are formidable and wealthy and, at best, successes will be compromises that will take many years to accomplish. We can't wait that long! Therefore, our best opportunity is to develop a system/program that will be quickly recognized to be superior to those that are currently available. To achieve this, I have the following observations and recommendations:
A bold goalThe proposed program will require significantly greater resources to provide equitable compensation for participating pharmacists than is provided by the current programs administered by PBMs. However, in considering the billions of dollars that are presently extracted from prescription plans by PBMs for their "services" and profits, I am confident that the proposed program will not only have better and safer outcomes for patients, as well as equitable compensation for pharmacists, but also will be provided more efficiently.Recognizing my personal lack of expertise and experience with respect to the development and operations of a pharmacy benefit program, I spoke with a pharmacist friend who has administered such programs. I asked him if my dream of our profession developing a program that would be competitive in recruiting Anthem as a client when its contract with Express Scripts concludes in 2019 was realistic. He promptly responded that he considered this realistic and I am emboldened to identify this as a goal. There will need to be earlier localized and incremental steps, the first of which is to establish the task force of experts! Daniel A. Hussar
|
|
| |